Content Warning:
This showcase presents a service that is for children and young people who have attempted suicide, have suicidal thoughts or have intentionally self-harmed which might be distressing for some people. We encourage anyone who is affected by this article to reach out for support. If you’re unsure where to go or who to reach out to, we recommend reaching out to Lifeline 24/7 crisis helpline 13 11 14 or any one of the following services.
The Royal Commission's into Victoria’s Mental Health System's Interim report, released in November 2019, identified a gap in suicide prevention service for children and young people at risk of suicide and self-harm. The Royal Commission recommended that the Victorian Government fund Royal Children's Hospital, Monash Children's Hospital, Alfred Health and Orygen to work in partnership to create, deliver and evaluate the first phase of an aftercare service for children and young people who have attempted suicide, have suicidal ideation or have intentional self-harmed.
The Royal Commission stipulated that the new Child and Youth aftercare service be informed by the experiences of children and young people as well as their families and carers, and by the program guidelines of the existing Adult aftercare service known as the Hospital Outreach Post-suicidal Engagement (HOPE) program.
The HOPE program is a core component of Victoria’s suicide prevention framework 2016-25, which aims to halve Victoria’s suicide rate by 2025. It is a psychosocial and clinical support service that delivers responsive outreach to individuals following a suicide attempt or are considered who are at significant risk of suicide with serious planning or intent and/or repeated intentional self-harm. HOPE teams support individuals and their personal support networks (family, friends and other carers) for up to 3 months helping them to identify and build protective factors against suicide.
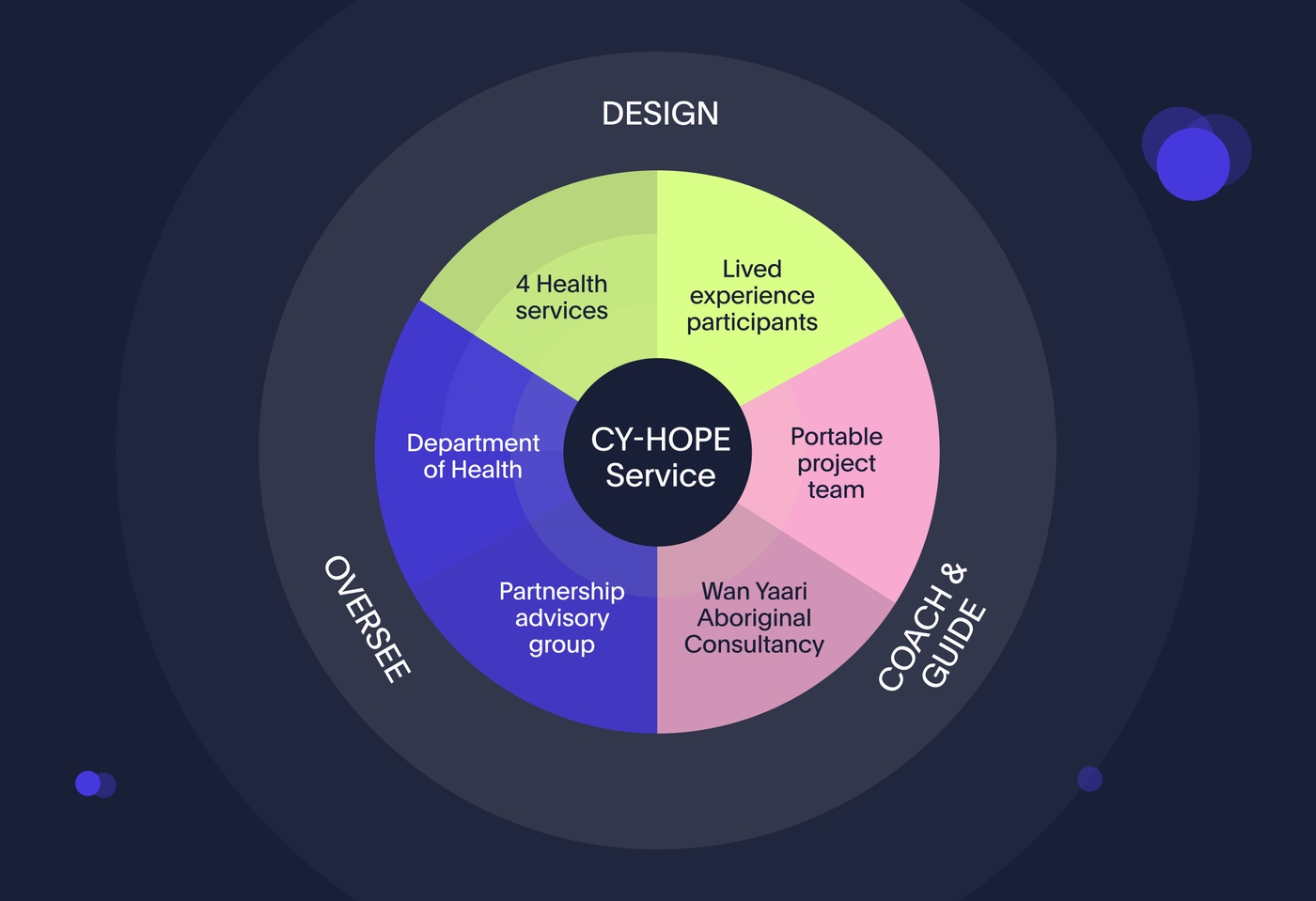
The Department of Health (the Department), which is responsible for implementing recommendations from the Royal Commission, funded 4 health services (Royal Children’s Hospital, Monash Children’s Hospital, Alfred Health and Orygen Youth Mental Health) to co-design a new Child and Youth Hospital Outreach Post-suicidal Engagement (Child and Youth HOPE) service and Portable was selected as their chosen supplier to guide them through this important process.
Design challenge
The project saw health services co-designing the new Child and Youth HOPE service with young people who have lived experience of receiving mental health support after self-harm, suicidal thoughts or a suicide attempt, and their carers and families (referred to as ‘lived experience’ throughout). Through this process, the health services and the Department sought to understand:
- The experiences of young people and their carers and families when receiving mental health and practical support after self-harm, suicidal thoughts or a suicide attempt, including what has worked and what hasn’t from their perspective.
- The service expectations of young people, their carers and families for a new Child and Youth HOPE service, the core characteristics of the service and the experience they wish to have.
- How a prototype of the service aligns with their expectations – what is working and not working and how the early model needs to change before the service is piloted.
The 4 health services were experienced in service design with differing levels of experience with co-design. Portable was engaged to build co-design capability at services with less experience and to support each health service in using a consistent approach to co-designing their local Child and Youth HOPE service, in partnership with children, young people, their families, carers, clinicians and service providers.
Approach
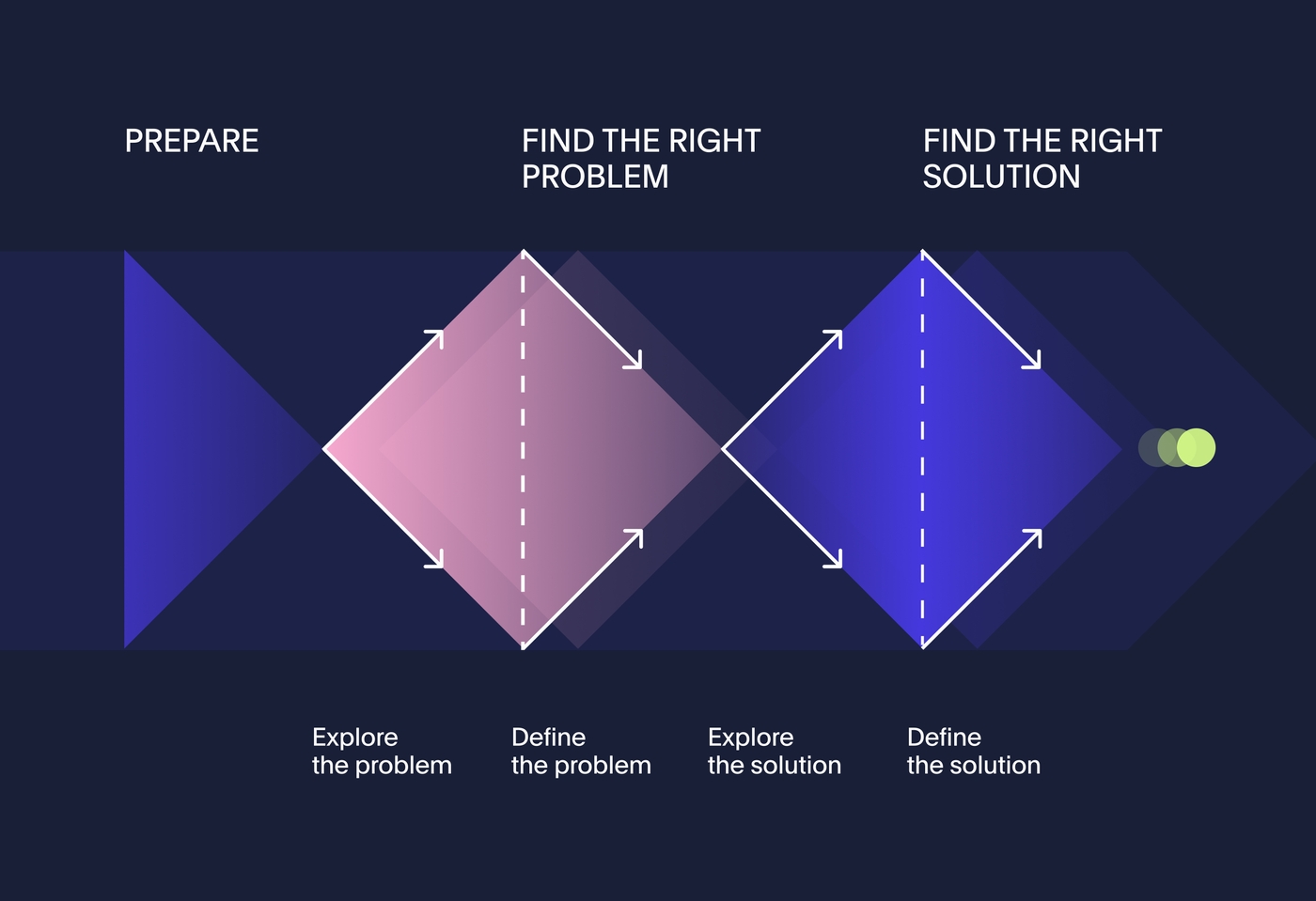
Starting with a 2-day foundational co-design training course, we introduced the Department and the health services to key concepts with a practical application of design activities. The training also included mindsets for social co-design, Portable’s mental health design principles and ethical considerations for power-sharing and participant safety.
We then individually coached the health service design teams through each stage of the co-design process, to support them in designing the service with people that have lived experience. Coaching at each stage included:
- Exploring the problem: Health services immersed themselves in the experiences of those they are designing the Child and Youth HOPE service with. They used a range of methods and activities to gain a deep understanding of those with lived experience and those who provide professional support, including workshops, contextual interviews and emergency department data analysis.
- Defining the problem: Health services organised all their findings and grouped them together in related themes and ideas. This is when they started to build a picture of the current end-to-end journey people go through and what they need at each stage in order to feel supported.
- Exploring the solution: We encouraged lived experience participants, lived experience leads and health service staff to be as imaginative and unrestricted as possible in their thinking at this stage, so that they could explore many possible ideas for solving the problem. Potential ideas for the new Child and Youth HOPE service were distilled into a concise and formulated concept, visualised as a prototype.
- Making the solution work: As teams moved through the co-design process they identified constraints, assessed and prioritised their ideas to refine the prototype that would balance what was desirable, viable and feasible. Health services tested and iterated their prototype until it was developed enough to inform a final Child and Youth HOPE Model of Care.

Safe and inclusive co-design in the mental health sector
Co-designing services with those who have lived experience is a growing practice in the mental health sector but it is not systemic.
For the Child and Youth HOPE project, all health services employed lived experience leads in their design teams, who worked alongside clinicians and other service providers as equal members of the local co-design team. This required clinicians and managers to broaden their perspectives, practice sharing power, balance the needs of each group and create a safe and ethical approach to participation.
Given that the Child and Youth HOPE service is for young people who have self-harmed or are at risk of suicide, this project tackled complex, traumatic and systemic problems that can be difficult and distressing for people to talk about with others. It was vital to create a safe space for people to share their experiences with confidence and trust so that the process of co-design wouldn’t cause further harm. Our approach to ensuring participant safety included:
- Health services invited and screened people with lived experience to ensure participants were ready to engage in co-design
- Psychological, peer and cultural support was provided to participants before, during and after co-design sessions.
- Clinicians and lived experience leads designed activities from a trauma-informed lens to reduce the risk of activities distressing people.
- Young people, families and carers were thoroughly briefed and gave informed consent before participating
Embedding lived experience into the team
Across the 4 health services, we co-designed with a broad range of people who have lived experience of the mental health system. This included 24 carers, 20 young people, 7 children, 28 clinicians, external service providers including education institutions (public, independent, alternative), a primary school nurse, Headspace, and health service stakeholders including NDIS Leads, Aboriginal health services, and refugee health services. Lived experience included representatives from the following groups:
- Aboriginal & Torres Strait Islander people
- Trans and gender-diverse people
- LGBTIQA+ people
- People with experience of family violence
- People with experience of the justice system
- Neurodivergent people
Effective partnerships
Portable partnered with Aboriginal consultancy Wan Yaari as cultural experts for the project. Wan Yaari provided coaching and consultation to the health service design teams, advising on facilitating co-design activities with young Aboriginal people in a culturally safe way and helping to ensure the Child and Youth HOPE Models of Care would be culturally appropriate and consider the needs of Aboriginal and Torres Strait Islander young people and families.
We also engaged with agencies on the Department’s Partnership Advisory Group (PAG) who provided additional representation for the voices and lived experiences of marginalised groups at greater risk of suicide. This included representatives from organisations that advocate for young people, children in out-of-home care, Aboriginal & Torres Strait Islander, migrant & refugee, neurodivergent, trans and gender diverse, intersex, and LGBTQI+ young people. The PAG was engaged at various points throughout the co-design process to highlight the main challenges facing young people in their communities, and to provide feedback on the health services Child and Youth HOPE prototypes. This has opened up conversations and pathways for the health services to continue engaging with these groups for further input into their service models and Child and Youth HOPE staff training programs.
Outcomes
Better lived experience representation in Victoria’s mental health system
Portable’s co-design support, coaching and capability building has helped the Department and the health services to understand and advocate for the value of lived experience expertise in their Child and Youth HOPE models of care. As a result, lived experience peer support roles working alongside clinicians are now central to all 4 Child and Youth HOPE models. All 4 health services have now launched a Child and Youth HOPE service. The co-design process allowed teams to create feedback loops to continuously improve the Child and Youth HOPE model of care, and this will be built into the service as teams apply the co-design mindsets and practices they learned during the project.
In addition to the relationships that the health services teams have built with each other, new relationships have been fostered with community organisations representing groups at greater risk of suicide through the Partnership Advisory Group (PAG).
This project has had a positive impact on the Child and Youth HOPE models of care, as well as broader health services and systems, paving the way for greater lived experience representation and safe co-design practise in Victoria’s mental health system.
Co-design capability uplift for health services
The health service design teams have gained valuable experience in the co-design process and are now sharing best practice more broadly. Insights from this project are also being shared more broadly with other teams in the health services (for example, with Emergency Departments). Health services are now considering how their new co-design practices can be integrated to improve other services.
Portable embedded regular reflective practice into the co-design coaching model, both with individual teams and across the health services. Collaborating across the Department and the 4 health services to share and amplify learnings created a mini-community of practice. Teams appreciated the opportunity to share and learn from one another. The Department facilitated weekly informal gatherings for the health services to share their progress, learnings, questions and concerns. This reflective practice is continuing as teams refine and implement their models of care.
Reflections
Young Lived Experience Co-Designer, Royal Children’s Hospital team
“There's a magic of giving a voice to people with those experiences because it's legitimising a mental health voice, or mental illness voice. It's almost breaking the stigma that we can't do these things and that we can't contribute. It gives a level of being able to speak from literal experience, as opposed to just assumptions.”
Olivia Gregory, Senior Producer
“In your career you’ll have projects that you connect with on a deeper level and always remember, and the Child and Youth HOPE project is just that. The impact this project will have for years to come is so significant and has been personally rewarding for the team to be part of it.”

CY-Hope has since been awarded Gold in the 2022 Melbourne Design Awards and Silver in the 2023 Australian Design Awards.
BETTER FUTURE (previously known as DRIVENxDESIGN) have awarded CY-Hope Gold in the category of 'Service - Government' at the 2022 Melbourne Design Awards and subsequently Silver at the 2023 Australian Design Awards. This category recognises "creative and innovative solution design for the successful delivery and provision of services. Consideration given to system integration, user experience, product design.”
We are delighted that our work in facilitating user-centred design to the mental health sector has been recognised in this way and we'd like to thank all of those involved in the project and setting it up for success. We hope that this helps promote the systemic need for co-designing services with those who have lived experience to ensure that new developments both align with the expectations and successfully offers services which meet the needs of those seeking much-needed support.
Project team
Olivia Gregory - Senior Producer
Jude Walta - Senior Design Strategist
Belinda Donald - Senior Design Strategist
Emily Pearce - Senior Content Strategist
Ryan Thompson - Senior Design Strategist
Cristiano Fantasia - Senior Experience Designer
Joanne Osbourne-Taylor - Lead Design Strategist
Ashlee West - Experience Design Lead
Allison Snow - Lead Producer